Social Entrepreneurship Accelerator

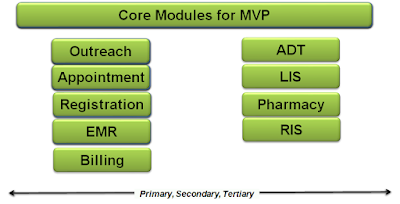
Social Entrepreneurship Accelerator [SEA] OpenHealthCODE is a a not for profit think tank working on NDHB Digital Health Standards for India. We run a Social Entrepreneurship Accelerator [SEA] for helping Indian HealthTech startups and vendors to implement Open Digital Health Standards that are applicable globally. #AtmaNirbharBharat #VocalForLocal SEA Silver Club Silver Club has implemented the Standards and achieved our Stamp of Confidence . https://openhealthcode.blogspot.com/2021/07/stamp-of-confidence.html SEA implements the eObjects Interoperability framework. eObjects were first written by Prof Dennis Streveler and Dr Pankaj Gupta in a white paper in Nov 2018 that was published by Niti Aayog in the book Health Systems for New India, Chapter 5 - Reimagining India's Digital Health Landscape Wiring the Indian Health Sector in Nov 2019. SEA Objectives SEA Cohort 1 SEA Cohort 2 In late October 2020, India's National Health Authority' Market ACCESS Program [MAP] put 12